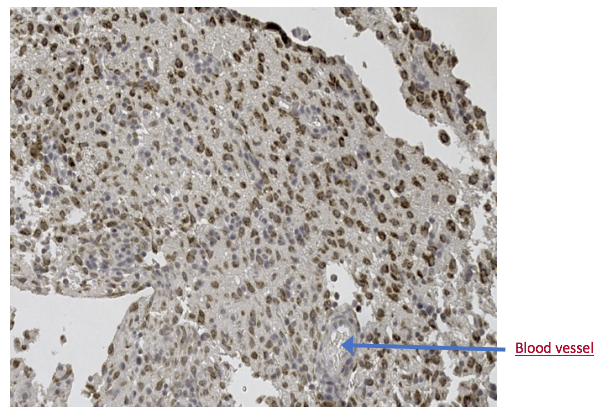
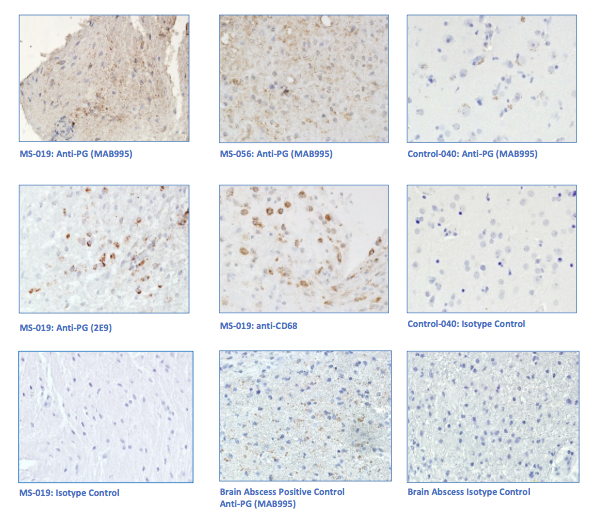
“primary demyelination” brain specimens from MS patients are full of macrophages, and that these macrophages appear to be “activated.” Macrophages—which start as monocytes in the bone marrow, move into the blood, and are recruited into areas of infection or damage--are a mop up team. And luckily for us in MS research, macrophages also work as antigen presenters. That is, they are drawn to areas of infection, they engulf and digest the offending microbes, and they “present” pieces of these microbes to the immune system. While macrophages can also be found in areas of damaged tissue, say after a crush injury or a burn, our interest lay in the macrophages in MS brain lesions. Figure: Macrophages stained within an MS lesion. Most experts in the MS field believe macrophages are bad news. They say that macrophages are drawn into MS brain lesions by the autoimmune process where they serve to damage tissue, harming people and doing no good at all. Because bacteria are not present, traditionalists hold, the macrophages must be a guerrilla SWAT team bent on brain destruction. (If this were true, scientists should be able to limit tissue damage and demyelination in patients by inhibiting macrophages, resulting in improvements in MS. However, drugs acting directly against macrophages have never been developed and tested, so we don’t know what their effects might be.) But my team and I wonder: What if macrophages are just doing what they are supposed to do—getting into infected areas to clean up and stimulate the immune system for a lasting fix? What if they are not the problem but, rather, a part of the solution? A special technique called immunohistochemistry has helped us see the bacteria—or at least parts of them—in MS brain lesions. Here’s how the science works. Peptidoglycan (PG) is an important component of bacterial cell walls. PG isn’t found in human cells. In fact, the human body raises up a special antibody against bacterial peptidoglycan. This “anti-PG” antibody binds to areas where peptidoglycan is present, so we can use it to detect the presence of PG in tissue, blood, or spinal fluid. In a convoluted series of steps, involving anti-PG antibodies and a few chemical cohorts, we can visualize PG on a slide. As with any good lab work, a set of controls proves that the reaction we see really is detecting bacterial peptidoglycan in human tissue. We tested as many MS brain samples as we could for PG using this method, called immunohistochemistry. We did not have too many samples to use because MS brain biopsy samples from living patients tend to be few. All four MS samples tested were positive for PG, with a much different pattern of PG reactivity seen in the epilepsy controls. Our group was not the first to apply immunohistochemistry to detect PG in MS brain lesions. Jon Laman from the Netherlands and Chris Power from Canada have also done it. In fact, we borrowed one anti-PG antibody from them, and bought another from a commercial supplier. Small groups of dedicated researchers are exploring the MS question as thoroughly and deeply as we can. We work together. We seek funding as well as scientific support for ground-breaking MS insights. If you’d like to take a look at bacterial peptidoglycan within MS brain plaques, you can get your science nerd on below. Figures: Immunohistochemical Analysis of MS Brain Tissue. These six photomicrographs show formalin fixed, paraffinized brain tissue sections from MS subjects, epilepsy controls, and a deidentified brain abscess control. The reddish or brown color shows detection of bacterial peptidoglycan (PG). Brain tissue from subject MS-019 shows specific staining with two different anti-PG antibodies. PG signal is also seen in MS-056 and faintly in epilepsy control subject 040. (The images are adapted from our February 4, 2019 article in Scientific Reports.)
So, in conclusion, and within the constraints of time, research funds, and available tissue samples, macrophages are in MS brain lesions and so is one important component of bacteria – peptidoglycan. The team showed previously that most MS brain biopsy specimens contain bacterial sequence different from the controls (read the sequencing blog here). So the scenes of the crime in MS patients’ brains contain bacterial RNA, bacterial cell walls (PG), and macrophages (either responding appropriately or causing trouble). Can we ever tell what really matters? Yes, we can, by measuring immune responses within the spinal fluid and blood. If those bacteria in MS brain samples are the root of trouble, macrophages will present them to the immune system. B lymphocytes and specific antibodies against those bacteria will be made in the brain and will collect in the spinal fluid. Which is the topic of our next blog: how the team grows bacterial candidates in lab culture, and what results that lab work has already delivered.
0 Comments
|
AuthorDr. John Kriesel is Associate Professor of Infectious Diseases at the University of Utah School of Medicine. He began this blog to raise awareness and generate discussion about the possible causes of multiple sclerosis. Archives
March 2021
Categories |
 RSS Feed
RSS Feed