|
Let’s do a 2021 roundup, a roundup of what we already know about MS, and what we hope to learn about this disease.
Here are the most important things we already know about MS (established facts):
Notice that MS is not identified here as an “autoimmune” disease. While many persons in the field believe that MS is an autoimmune disease, no clearcut “autoimmune antigen” has ever been identified. The current enthusiasm among scientists for myelin, for instance, as the target of the immune system in MS must be tempered by the realization that the oligoclonal bands (antibodies) in the spinal fluid of MS patients generally do not target myelin. More on this subject later . . . Here are the things we have shown in our lab, and can be relatively sure about (i.e. additional facts):
These two things – overexpressed microbial sequences and spinal fluid antibodies against some of these microbes – make us much more enthused about the idea that microbes might be causing MS. Here are some things we don’t know, but would like to find out:
Thought Experiment – The Hot Pepper Let’s think about MS in a different way, starting with a “thought experiment.” This is a hypothetical experiment that we just think about and never actually perform for reasons which will become obvious. Einstein used to do thought experiments to illustrate a point. As my family, friends, and colleagues will tell you, I am no Einstein, but let’s try this anyway. Suppose I have a hot pepper. Maybe a jalepeno or habanero, but really hot. And it doesn’t really matter if the pepper is freshly picked and still alive, dead and dried out, or crushed, the result will be the same.
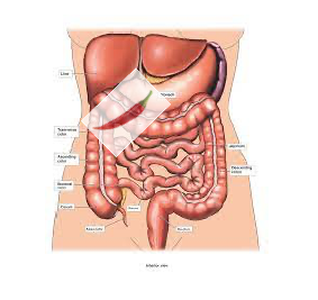
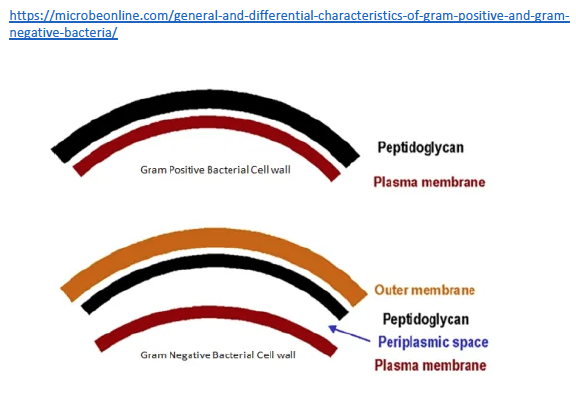
And maybe this will work if it’s small enough to be easily eaten (phagocytosed) and removed. But if it’s large enough, the macrophage removal process will not be enough, and that pepper will fester. Surrounding tissue will be damaged and destroyed, and our unfortunate patient will have chronic pain, organ dysfunction, and maybe even perforation of the adjacent bowel (not good). So how is this even remotely relevant to MS? Well, it is relevant because those microbial sequences we found in MS brain tissue are attached to their own little hot peppers. That is, they are made of microbial proteins, including one class that is really irritating – peptidoglycan. Peptidoglycans give bacterial cell walls their structure. Without them bacteria fall apart. And peptidoglycans are irritating, dead or alive. The immune system of animals and humans has evolved to detect and eradicate peptidoglycans.
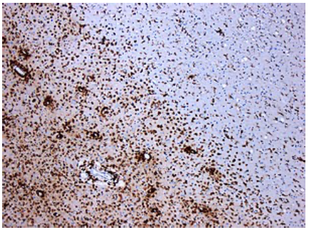
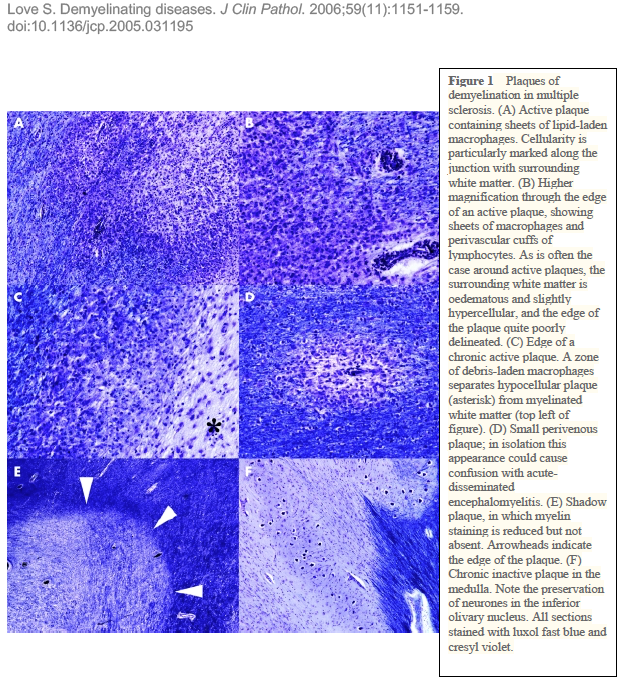
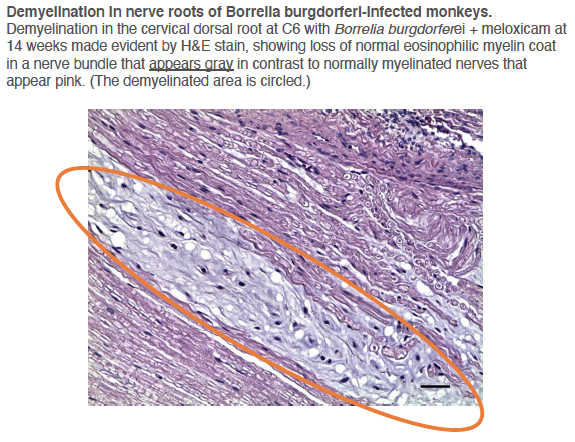
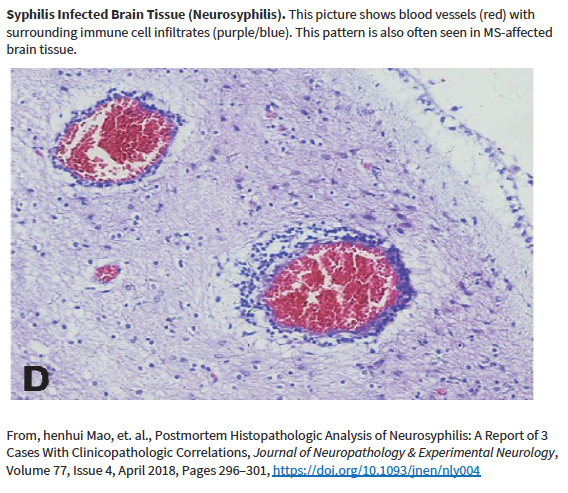
Other researchers have shown specific antibodies against bacterial peptidoglycans in the spinal fluid of MS patients. When we took our MS candidate bacteria (identified by sequencing MS brain lesions) and sonicated them, their peptidoglycans were exposed. Therefore, we likely detected antibodies against peptidoglycans in the spinal fluid of MS patients. That is, MS patients are making an immune response to bacteria and bacterial peptidoglycan in their spinal fluid. It may not matter if the bacteria are alive or dead, whether they arrive from the bloodstream or from infiltrating macrophages, their presence (and their peptidoglycans) are doing evil. The Microbial Hypothesis of MS It’s hard to imagine that bacterial antigens (proteins), including peptidoglycan, in the brains of patients with MS are doing anything but raising havoc – inflammation, macrophage infiltration, and the destruction of an important bystander, myelin. That’s right, our view at Cracking the MS Code is that the MS disease process does not specifically target myelin. It targets bacteria and their antigens within brain tissue, and myelin is damaged in the process. Myelin is a bystander, injured by the inflammatory process surrounding it. If the bacterial antigens are removed quickly and completely, myelin and their enveloped axons may be preserved without any loss of function. If there is some damage to myelin, remyelination may occur. But if all the bacterial antigen cannot be removed, or if new bacterial antigen is formed due to replication of bacterial cells, the inflammation goes on, myelin is ruined and removed, axons are lost, and neurologic deficits ensue. Neurosyphilis, Neuroborreliosis, and Neurologic Tuberculosis MS is not the only disease with oligoclonal bands (OCBs) appearing in the patients’ spinal fluid. Neurosyphilis, syphilis that affects the brain or spinal cord, and neuroborreliosis, neurologic Lyme disease, are bacterial diseases that bear some resemblance to MS. Both of these bacterial infections can be insidious and chronic. Both often cause OCBs to form in the spinal fluid. However, the OCBs are directed against the infecting bacteria, not myelin. (Remember, these OCBs are really IgG antibodies made in the brain and/or spinal cord, so, of course, they are directed against the invading microbes.) And both neurosyphilis and neuroborreliosis (neurologic Lyme disease) can cause severe neurologic dysfunction and death. These bacterial brain infections can relapse even after treatment. And in neither disease can the causative bacteria be cultured directly from the spinal fluid. Diagnosis requires special serologic or molecular testing of the blood and spinal fluid. Neurologic Lyme disease is inflammatory and can cause demyelination. The pathology of affected brain and spinal cord resembles MS in several ways, including the presence of demyelinated areas. The demyelinated area is circled (DOI:https://doi.org/10.1016/j.ajpath.2015.01.024) Neurologic tuberculosis is also interesting. This disease is “paucibacillary” (few bacteria). That is, a very few tubercle bacilli cause a terrible disease that is difficult to diagnose and hard to treat. Diagnosis requires culturing large volumes of spinal fluid for weeks or months to find the causative tubercle bacilli. If you catch them, you are lucky. Treatment is often started empirically (by a guess), and stopped later if all tests are negative. And treatment of neurologic TB requires suppression of the immune system to lessen the damage. These cases are treated with a combination of anti-tuberculosis drugs and steroids, usually prednisone. Months of treatment with these antibiotics and a slow taper of the steroids is required to control and cure the disease.
I offer this for your consideration because I want to see the bigger picture with MS: What if MS is also a “paucibacillary” disease, usually caused by bacteria, a few or many different ones, that cannot be easily cultured from the spinal fluid, that may lay dormant and recur, and that must be diagnosed indirectly by serology? Our lab at Cracking the MS Code aims to show that spinal fluid serology tests are the most effective way to diagnose and direct the treatment for developing MS. If this proves to be true, doctors could make early diagnoses and apply appropriate treatments including antibiotics to suppress or eradicate the inciting bacteria, with specific immunosuppressants to minimize the damage. Can we actually cure cases of MS? I think this is possible, but we need to know exactly what we are facing. Guessing is not acceptable. Next article: Who should we treat, and how can we do it? What are the chances of making these patients better or limiting the neurologic damage?
0 Comments
Your comment will be posted after it is approved.
Leave a Reply. |
AuthorDr. John Kriesel is Associate Professor of Infectious Diseases at the University of Utah School of Medicine. He began this blog to raise awareness and generate discussion about the possible causes of multiple sclerosis. Archives
March 2021
Categories |

 RSS Feed
RSS Feed